For World Cancer Day we are taking a look at a new study into liver cancer rates across Europe and the UK.
Liver cancer related deaths in Europe rose by 70% between 1990 and 2019. But there are big differences in the numbers between and within countries. The new study, in the Journal of Hepatology, looks at reasons for this, and suggests what could be done.
Liver cancer is almost always caused by long term liver disease. There are many causes of liver disease but the most common are viral hepatitis, drinking too much alcohol, and being overweight. People often have liver disease for many years before realising there is a problem. This damage might not be noticed until someone has advanced cancer that cannot be treated.
There are ways to prevent, find, and treat liver cancer. But these opportunities are often missed.
Liver cancer rates and deaths are increasing across Europe.
The study looked at liver cancer rates across the European Economic Area and the UK.
Viral hepatitis has always been a big cause of liver cancer. It is still a problem in countries where it is hard to get hold of vaccines or treatment. But in many countries, it is now causing fewer cancers.
Unfortunately the overall number of liver cancers is going up. This is being driven by increases in alcohol and diet related liver disease.
There are also big differences within each country.
Vulnerable and marginalised groups are most at risk
The study found that people in vulnerable or marginalised groups were more likely to get liver cancer and more likely to die from it.
What makes a group of people more vulnerable is complicated and is different for different groups.
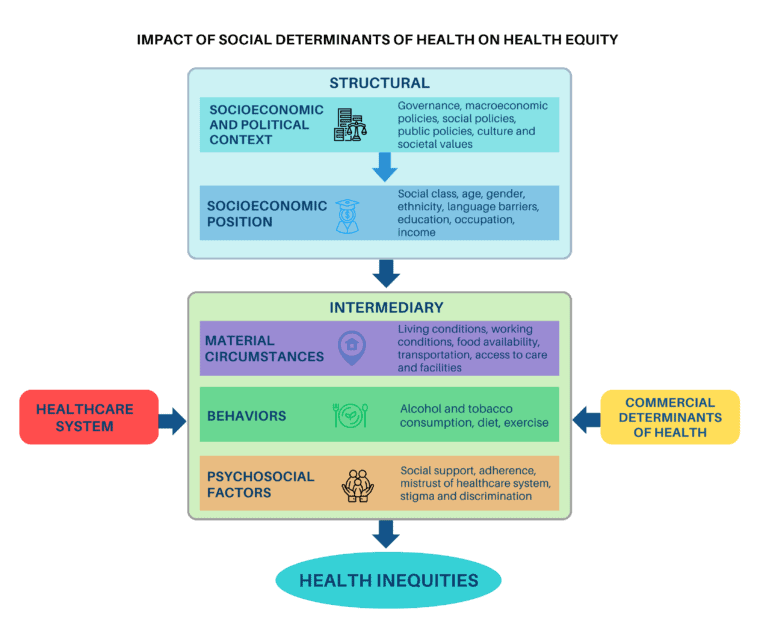
The study divides the issues into:
- Structural issues
- E.g. education, language barriers, government policy, social norms
- Intermediary issues
- E.g. living conditions, diet, social support, access to transport.
All these things also interact with each other. In ways we do not yet fully understand.
Risks build up in vulnerable groups
It takes a long time to go from risk factors to liver disease, to liver cancer. But vulnerable people have an unfair disadvantage at every stage.
The first problem is that people in vulnerable groups are more likely to have a liver condition that can cause cancer. And less likely to get treatment for that condition in time.
One example is hepatitis C. Without treatment, hepatitis C carries a high risk of liver cancer. But 9 in 10 cases can be successfully treated. This reduces the risk of getting liver cancer by 70%. But it is harder for people in some vulnerable groups to get treatment.
People at risk of liver cancer can have a simple scan to find it early. But in Europe less than a quarter of liver cancers are found this way. Stigma is a big part of the problem and is often directed at vulnerable groups. Fear of shame or judgement, particularly around alcohol or obesity, stops many people from seeking help. So they are not referred for a scan.
The study found that people with undiagnosed alcohol or diet related liver disease are most likely to miss out on vital scans.
Finally, when cancer has been diagnosed, it is vulnerable people who are most at risk of dying.
Again there are many reasons for this. People may be diagnosed later when their condition cannot be treated. Or they could struggle to get to treatment appointments if they live far away and have a limited budget.
We can tackle liver cancer
The health inequalities causing much of the liver cancer across Europe are deeply unfair. But they are also avoidable.
At the moment, much of the research into liver cancer is focused on treatments. The authors of this paper suggest we also need a better understanding of the social issues that stand in the way of prevention, diagnosis, and treatment.
They call for more research into these health inequalities so that we can find out how they affect different groups and how they interact with each other.
This information can help services to adapt to ensure those most in need are able to access them. This could take many forms, for example taking a screening clinic out to a high-risk community. Or designing better information that will work for a group who really need it.
We also need to change attitudes to liver disease. The stigma surrounding alcohol, obesity and viral hepatitis stops people seeking the help they need until it is too late. It is even a barrier for those whose liver condition is not related to any of these things.
Stigma is also part of another problem identified in the paper. Compared to a lot of other cancers, liver cancer and liver disease are not talked about. This lack of awareness is also stopping many people from coming forward for tests and from making changes in their life that could prevent cancer.
Liver Cancer UK and The British Liver Trust are working to improve access to early diagnosis and to understand and tackle stigma. You can read more about this work on the British Liver Trust website by using the links below.
