Stage D HCC means you are very unwell and need help looking after yourself. This may be because your liver is very damaged either from the cancer, or from other liver disease.
The liver is important in processing toxins, including medicines. If you have stage D HCC, it means your liver is not working at all well. Because the treatments for HCC can be quite difficult to cope with, your body is unlikely to be able to withstand them. So your doctor is likely to suggest that you have treatment to try and control your symptoms and help you feel better. This is sometimes called palliative care – palliation means relief of symptoms.
There is information about controlling symptoms of advanced liver cancer in our general info on liver cancer treatment. This tells you about medicines you may have to help control any pain or sickness. Your doctor may also recommend any of the following treatments:
- Radiotherapy
- Treatment to remove fluid from your tummy (abdomen)
- A stent to help with jaundice
Radiotherapy
HCC can sometimes spread to the bones and cause pain. If this happens, your doctor may suggest radiotherapy. This generally works well for relieving bone pain. You are most likely to have a single treatment. Or you may have a few treatments over a few days.
There is more about radiotherapy in the general info on liver cancer treatment .
Treatment to remove fluid
With liver disease, people sometimes have fluid building up in their tummy (abdomen). The liver normally makes proteins that hold water in the bloodstream. Without these, fluid can leak out and collect in your abdomen, causing swelling. This can be very uncomfortable and cause shortness of breath if the fluid is pressing upwards into the muscular sheet under the lungs (the diaphragm – say: dye-a-fram).
Your doctor may suggest relieving the pressure by draining some of the fluid. They may call this a ‘tap’ or abdominal paracentesis (say: para-sen-tee-sis). After a local anaesthetic injection, the doctor puts a small tube through your skin and into your abdomen. The tube is connected to a drainage bag and the fluid allowed to drain away.
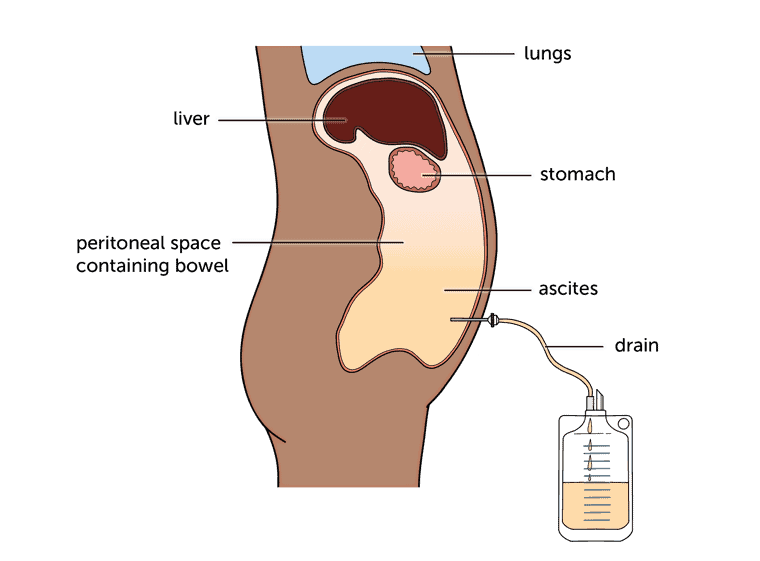
Your nurse will make sure the fluid drains quite slowly. If it’s too fast, it can affect your blood pressure and make you feel faint. How long the tube stays in depends on how much fluid needs to drain. It’s usually a few hours, but may be overnight.
The fluid will build up again after a while. You may have water tablets (diuretics) to try and slow it down. Or your doctor might suggest leaving the tube in permanently so you don’t have to keep having the procedure repeated.
A stent to help with jaundice
Jaundice (say: jawn-diss) is a common symptom in advanced liver disease. You may have it in liver cancer because a tumour is blocking your bile ducts. Bile salts build up in the body, making you feel very unwell and causing uncomfortable symptoms such as itching.
Unfortunately, in advanced HCC, you may have jaundice because your liver isn’t working properly, rather than because of a blocked bile duct. So this treatment doesn’t often relieve symptoms completely.
If they think it’ll help, your doctor may suggest putting in a small tube (the ‘stent’) to help drain bile. This is about as thick as a ball-point pen refill and 5 to 10cm long (2 to 4 inches). It holds a bile duct open so that bile can flow into the small bowel.
You may have a stent put in in through a small cut in your skin – a PTC procedure. There is information about PTC in the general info on liver cancer tests.
Stents usually need to be replaced every 3 or 4 months as they can become blocked, and cause an infection (cholangitis). If you have:
- high temperature (fever)
- your jaundice getting worse
- chills or shivering
contact your doctor or CNS (Clinical Nurse Specialist). Untreated, cholangitis can be serious. You may need antibiotics and a replacement stent.
Content last reviewed: October 2022
Next review date: October 2025
[LW5]LINK general liver cancer tests#PTC
[LW6]LINK liver cancer tests
