Chemotherapy is a treatment with drugs that kill cancer cells.
What chemo is
Chemo is sometimes called cytotoxic therapy, which means toxic to cells. Chemo drugs kill cancer cells while doing little harm to normal cells. The treatment circulates throughout your body so it will kill cancer cells wherever they are.
Both normal cells and cancer cells grow by dividing into 2 new cells. Chemo drugs kill cells that are in the process of dividing. Cancer cells divide and grow much more often than normal cells. So they are more likely to be killed by chemo drugs.
When you have chemo for liver cancer
For bile duct cancer or gallbladder cancer, you may have chemotherapy after surgery to try and cure your cancer. This is to lower the risk of the cancer coming back. Doctors call this adjuvant treatment (say: add-joo-vent).
For bile duct cancer, you may have chemo before surgery, to shrink the cancer before the operation to remove it. Doctors call this neoadjuvant treatment (say: nee-oh-add-joo-vent).
You may also have chemo for advanced cancer that has spread from where it started. Because chemo circulates throughout the body, it can kill cancer cells wherever they are.
For hepatocellular liver cancer (HCC) you may have chemo in a very different way. It’s part of a treatment called TACE. This is localised treatment given directly to your liver and has fewer side effects than regular chemo. There is more about TACE in this section.
How you have chemo
You most often have chemo either directly into your bloodstream through a drip (intravenous infusion) or by mouth, as tablets or capsules that you swallow. This depends on the particular drugs you’re having.
You usually have a course of treatment that lasts around 6 months. You have treatment for a week or more and then have a break before your next treatment. For example, you may have treatment for a week and then 3 weeks off before your next treatment. This will vary, depending on the exact course of treatment prescribed for you.
Common chemo side effects
Each chemo drug has a different set of possible side effects. But there are some that are common to many.
Because chemo kills cells that are dividing, side effects tend to affect body tissues with cells that are often replaced, including
- skin cells
- cells that line your digestive system
- cells in hair follicles.
At any one time, some of these cells will be dividing and so are more likely be killed by the treatment. The remaining cells survive and replace the missing cells. So the side effects will go once the course of treatment is over.
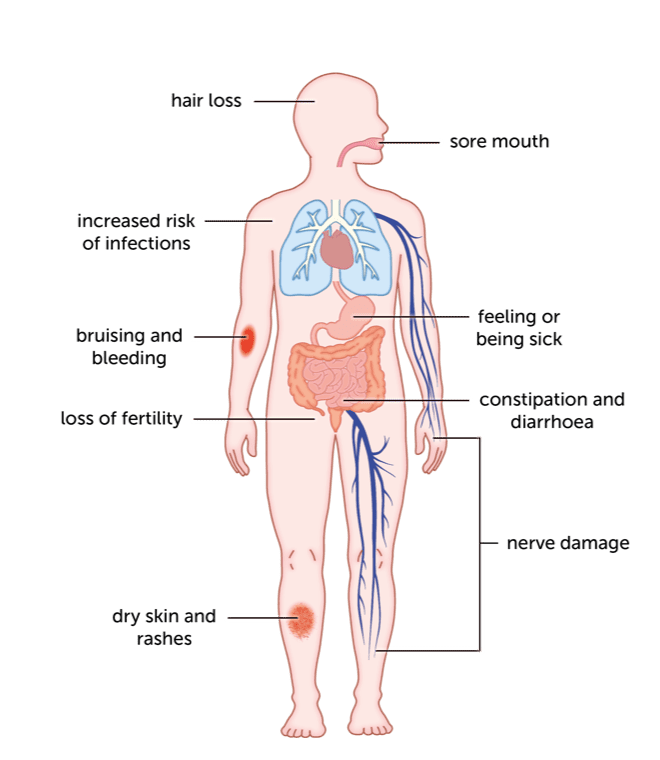
Common side effects include
- a drop in the number of white blood cells, increasing risk of infection
- a drop in the number of blood cells called platelets, increasing risk of abnormal bleeding (such as bruises for no reason, nosebleeds or bleeding gums)
- a drop in the number of red blood cells, causing tiredness and breathlessness
- sickness or diarrhoea
- hair loss or thinning
- sore mouth, mouth ulcers and changes in taste
- loss of fertility because of the effect on developing eggs and sperm
- dry skin, rashes and increased sensitivity to the sun
- nerve damage, causing pins and needles, pain or numbness in hands and feet
Side effects usually go in the weeks after you’ve finished your course of treatment. Some body tissues take longer to recover than others. For example, nerve damage can last for some time after you’ve finished treatment and can be permanent in a small number of people.
The effect on fertility may be permanent. If you are concerned about this, discuss it with your doctor before starting treatment. There may be different drugs you could have that are less likely to cause permanent infertility. Men may be able to bank sperm before their treatment starts.
Your doctor or nurse will give you information about the side effects of the drugs you’re having. Do tell them about anything you think may be a side effect. There are medicines that can help, for example with sickness or diarrhoea. If your side effects are too troublesome, your doctor may reduce your chemo dose or put your treatment on hold while you recover.
Clinical Trials
Cancers starting in the liver are not very common. So doctors and researchers across the country and internationally work together to find and test new treatments in clinical trials. Your doctor may suggest a trial that they think is suitable for you. Do ask them if you’re interested in finding out about trials you may be able to join.
We have more information about finding a clinical trial.
Content last reviewed: October 2022
Next review date: October 2025
