Advanced stage HCC means your Barcelona stage is C. This means that the cancer has grown into blood vessels. Or it has spread to lymph nodes (glands) or another part of your body. People in this group are still relatively well but you may be less active than usual. Your liver may be working normally or you may have moderate liver damage.
Your specialist is most likely to suggest treatment with a type of drug called a ‘targeted therapy’. The aim of this treatment is to try and control the cancer for as long as possible.
Targeted therapies
Targeted cancer drugs are the newest type of cancer treatment. Some of them may also be called biological therapies or biologics. There is more information about what targeted therapies are and how they work in the general info on liver cancer treatment.
Your doctor may suggest the following courses of treatment:
- A combination of drugs called bevacizumab and atezolizumab
- A drug called sorafenib
- Other targeted therapies], including drugs called lenvatinib and regorafenib
We have listed the most common side effects for each of these medicines. Remember that everyone reacts differently to treatment. Side effects can be mild in some people and more severe in others. You are very unlikely to have all the common side effects, but may have several. Let your doctor know about your side effects. They can help you manage them or may need to adjust your treatment.
Bevacizumab and atezolizumab
This is the most likely treatment you’ll have, providing your liver is working normally and you are well enough to do pretty much everything you normally do, except heavy physical work.
Atezolizumab blocks a protein that cancer cells make. This protein stops your immune system attacking the cancer. So it’s a type of immunotherapy.
Bevacizumab stops cancers from growing blood vessels. Cancers need nutrients and oxygen brought to them as they grow. So, blocking this blood vessel growth helps to cut off their food supply.
You have this treatment into your bloodstream, through a drip (intravenous infusion). You have to go to hospital chemotherapy department for treatment every 3 weeks. You can usually carry on with the treatment for as long as it’s helping you and you’re coping with any the side effects.
The most common side effects include:
- Diarrhoea
- feeling or being sick
- headache or aching joints
- tiredness (fatigue)
- numbness and tingling
- a drop in blood cells, increasing risk of bleeding and infection
- poor appetite
- an itchy rash
- a raised temperature
- a cough or shortness of breath
- changes in your blood pressure
- eye problems
- a sore mouth
Some people have an allergic reaction when they are having the infusion – tell your nurse if you have difficulty breathing, a rash or dizziness. Your doctor will give you steroids to damp it down.
Sorafenib
If bevacizumab and atezolizumab aren’t suitable for you, your doctor is most likely to suggest sorafenib. To have this treatment, your liver must be working normally.
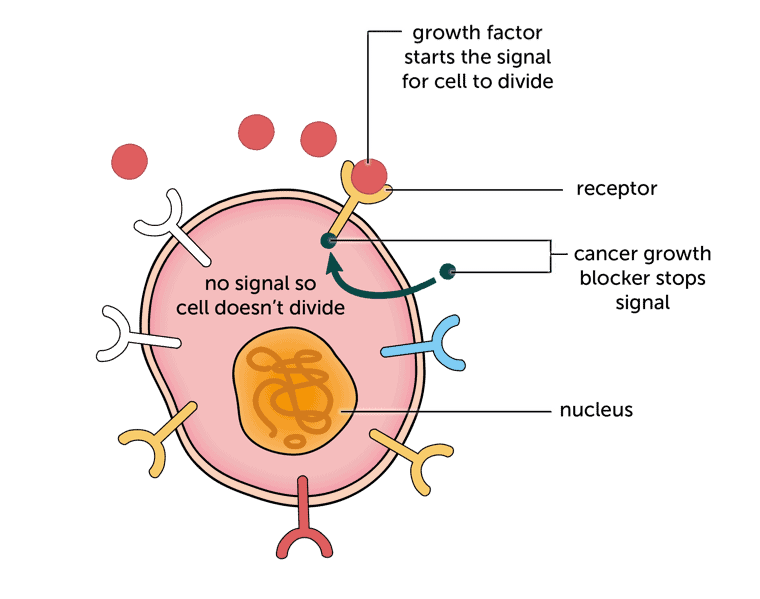
Sorafenib works by blocking chemical signals that tell cancer cells to divide and grow.
Like bevacizumab, it also helps to stop cancers from growing blood vessels. It is a tablet that you take at home twice a day on an empty stomach (either 1 hour before a meal or 2 hours afterwards).You continue to take the tablets for as long as they are helping you.
Sorafenib does have side effects. The most common include:
- diarrhoea or constipation
- feeling or being sick
- a rash, which may be red, sore or itchy, especially on hands and feet
- headache, aching joints or muscles or tummy (abdominal) pain
- tiredness (fatigue)
- poor appetite and weight loss
- a hoarse voice
- high blood pressure
- nosebleeds or other abnormal bleeding
- a sore mouth
Other targeted therapies
There are other similar drugs to sorafenib that you may have. These include lenvatinib and regorafenib. There may be other targeted therapies that your doctor suggests. We have only included those used most often here. They all have slightly different side effects. So ask your doctor to give you information about the particular treatment you are having.
Lenvatinib blocks chemical signals that tell cancer cells to divide and grow. It is a capsule that you can take at home. You take the capsules once a day. You can carry on taking them for as long as they are helping you.
Lenvatinib has the same common side effects listed above for sorafenib. It may also cause:
- difficulty sleeping
- hair thinning
- taste changes
Regorafenib also works by blocking cancer cells’ growth signals. It comes as tablets that you take once a day with a low fat meal (toast and cereal for breakfast, for example).
The most common side effects for regorafenib are the same as for sorafenib.
Content last reviewed: October 2022
Next review date: October 2025
