TACE stands for Trans Arterial Chemo Embolization. TARE stands for Trans Arterial Radio Embolization. TARE may also be called SIRT (Selective Internal RadioTherapy).
What are embolization, TACE and TARE (SIRT)?
Embolization means to block a blood vessel. In cancer treatment, doctors use it to block a blood vessel that is supplying a tumour. By cutting off its blood supply, the treatment is stopping food and oxygen getting to the cancer cells, so they die.
To treat liver cancer, doctors often use embolization with chemotherapy or radiotherapy.
TACE combines blocking off the tumour’s blood supply with a high dose of chemo directly to a liver cancer. So it’s a two-pronged approach. The chemo kills the cancer cells and blocking the blood supply cuts off the cancer’s food and oxygen.
TARE and SIRT are different names for the same thing. Instead of chemo, you have beads carrying short-acting radiation put in before the blood supply is blocked off. The radioactive source is shut in by the blocked blood vessels. The energy from the radiation only travels a few millimetres and wears out within a couple of weeks. So it delivers a high dose of radiation directly to the cancer without affecting the normal liver tissue too much.
When you have embolization TACE or TARE / SIRT
TACE and TARE are used for hepatocellular liver cancer (HCC). There are several situations when your doctor may suggest it:
- for early HCCs if you have several tumours in your liver
- alongside other treatments to try and cure early stage HCC
- to control a liver tumour while you’re waiting for a transplant
- to shrink (‘downstage’) HCC so you might be able to have a liver transplant
- while you are waiting for a transplant, to help keep HCC under control
- to try and control HCC that has come back (recurred) after earlier treatment
there is more about these in the information on HCC
How you have embolization
You have this treatment in hospital, in the radiology department. You usually need to stay in overnight. You have a sedative, so your nurse will ask you not to eat for around 4 hours beforehand. This is in case the sedative makes you feel sick. Check with your doctor about any medication you usually take – or if you are diabetic and not eating will be a problem. You can usually sip water, but check with your nurse before you do.
The treatment takes around an hour and a half. First, you need to have an angiogram. This means the doctor injects dye to show up the blood vessels in your liver.
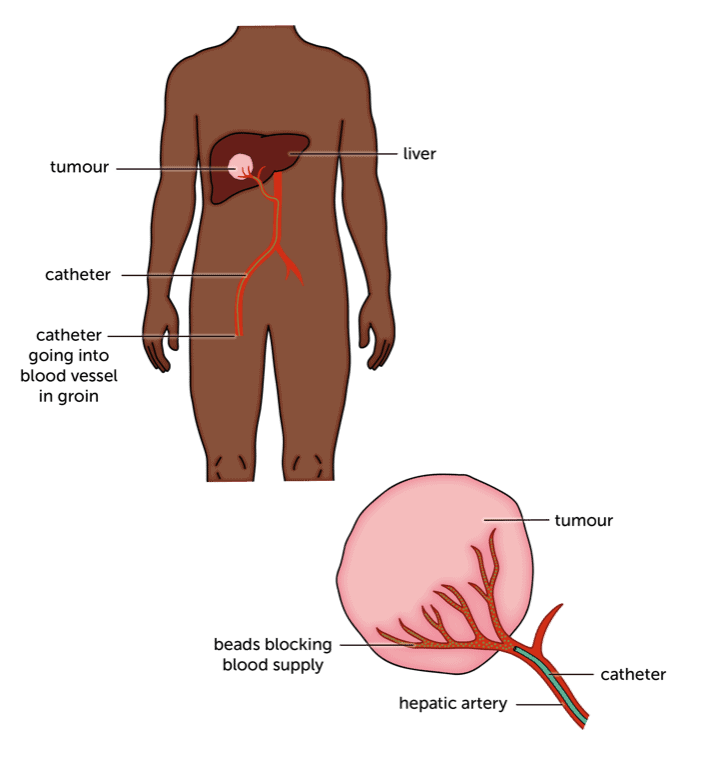
You can have a sedative to make you drowsy if you’re anxious. After giving you some local anaesthetic, the doctor makes a small cut in your wrist or groin. They thread a thin tube (catheter) in to the artery in your groin or wrist. Then they guide it through to the main artery supplying the liver (the hepatic artery). They use an X-ray to check where the catheter is going.
Once the catheter is in place, the doctor injects a dye so they can see the blood vessels in the liver on an X-ray.
The dye may make you feel hot for a minute or two – this is normal. The doctor will be able to see which blood vessels feed your liver tumour(s).
For embolization, the doctor then injects some microscopic beads before removing the catheter. The beads block these small blood vessels.
After taking the catheter out, the doctor will put a pressure dressing on the wound in your wrist or groin. If the wound is in your groin, you’ll have to stay in bed for 4-6 hours afterwards, to reduce the risk of bleeding (which is why you usually stay overnight). You can eat and drink normally once you’ve got over the sedative.
Having TACE
If you’re having TACE, you will have an angiogram, as for embolization. Once they’ve found the blood supply , the doctor will inject chemo directly into these blood vessels, followed by the beads. This seals in the chemo and at the same time cuts off the tumour’s blood supply. They may use chemo impregnated beads that do the job in one go (these are called drug eluting beads).
Recovery from TACE is the same as for embolization. Your doctor may do a scan around 4-6 weeks after your treatment, to see if the tumour has shrunk.
How you have TARE / SIRT
If you’re having TARE, you will have an angiogram a couple of weeks before your treatment. This is called a planning angiogram. It’s the same as having an angiogram for embolization or TACE.
The planning angiogram
After finding the tumour’s blood supply, the doctor will look for any blood vessels that could carry the radioactive beads away from the tumour. They’ll block these, so the beads won’t be able to escape.
Then they’ll inject a small amount of radioactive liquid. This shows where the beads can get to. It double checks that none will be able to travel in the blood stream to other parts of your body. Once the doctors are sure it’ll be safe for you to have TARE, they take the catheter out.
As with embolization, there’s a risk of bleeding after this test. You’ll have a pressure dressing on your wrist or groin. You’ll have to rest in bed for around 6 hours afterwards if you’ve had the catheter put into your groin. So you may be in hospital overnight.
Having the treatment
A week or two after your planning angiogram, you have TARE. This is the same as having your planning angiogram. But this time, the doctor injects the radioactive beads. It’ll take about an hour.
Recovery is the same as for the planning angiogram. If you need it, you can have medicines for pain or sickness. The next day, you’ll have a scan to make sure the beads have stayed in the right place.
It can take longer to see how well the treatment has worked than it does for TACE. You may not have a scan to check until 3 to 6 months after treatment.
Radiation precautions after treatment
The radiation from the beads will be gone in a couple of weeks. The beads are harmless and stay where they are.
The radiation is strongest for the first couple of days. Even though it doesn’t travel more than a few millimetres from the beads, there are a couple of precautions during this time. Your doctor may ask you to:
- wash your hands carefully after using the toilet
- avoid getting too close to babies or pregnant women
- sleep on your own for the first couple of nights after treatment
Embolization TACE and TARE side effects
The side effects you have are caused by the embolization, rather than any chemo or radiation from TACE or TARE.
You don’t usually have side effects from the chemo, as it’s blocked in the liver. Sometimes some of it can leak out and cause side effects. There is info about the most common side effects of chemo in this section. But do ask your doctor what to expect from the particular chemotherapy drug you’ve had.
The radiation in TARE only travels a few millimetres, so it doesn’t affect much normal body tissue and doesn’t tend to cause side effects either.
Most people have a raised temperature for a few days after any type of embolization. You may also:
- feel sick or have diarrhoea
- feel very tired
- have pain over your liver, which may spread up into your right shoulder
- have flu-like aches and pains
These side effects are caused partly by chemicals being released as cancer breaks down. They usually start within a day or so of having treatment and last for up to 10 days. Tiredness may carry on for a few weeks.
If you have any concerns about side effects, or they carry on for longer, contact your hospital. You should let them know if your temperature goes above 38°C, as that could mean you have an infection.
If the puncture wound in your groin becomes hot, swollen or red, you should also contact your doctor. You may need antibiotics.
Content last reviewed: October 2022
Next review date: October 2025
